A Valve for the Most Vulnerable
‘Star’ Ph.D. student helps develop medical device for children with congenital heart defects
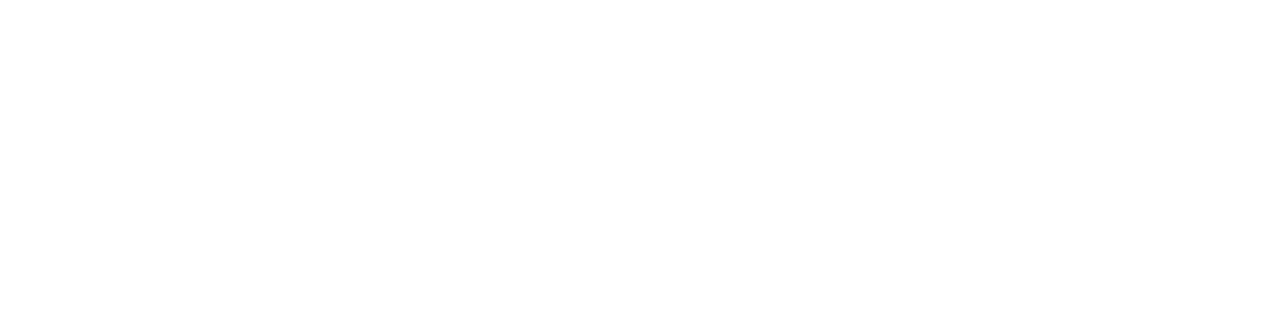
Dec. 11, 2024 - Nnaoma Agwu, a fourth-year Ph.D. candidate under the guidance of Professor Arash Kheradvar, M.D., Ph.D., in the Department of Biomedical Engineering, says he knew from an early age that he would pursue inventions to help people, and his experience at UC Irvine has confirmed that vision.
“Even my parents thought I was kind of a reckless kid, always taking things apart and putting them back together again,” Agwu says. “I definitely think the ‘mechanics’ aspect was a driver in getting me involved in mechanical engineering.”
Supplementing his at-home tinkering, he met an inspiring science teacher at his high school in Denver, where he first learned about ventricular assist devices and artificial heart pumps.
“I was fascinated that people had developed these machines that can help sustain others’ quality of life, and that made me think that maybe there would be an opportunity for me to go beyond designing cars or planes to doing something that could help patients,” Agwu says.
His time in the Kheradvar lab since 2021 has given him that chance.
Congenital heart defects
Every year, more than 1.3 million babies are born with congenital heart defects. Originating in the womb, these abnormalities can lead to constriction or blockage of blood flow near a heart valve that directs the flow toward the lungs. If not treated promptly, they could become life-threatening or significantly hinder children’s development.
But small and growing bodies present a challenge. Open-heart surgery is usually performed on infants to relieve valve narrowing. However, this procedure often results in a leaky valve, which can lead to even more serious health complications. And as babies grow, their hearts also grow, eventually rendering implanted medical devices obsolete.
“There are some products that are clinically available, but they are not indicated for children until they’re at least 20 kilograms, or about 44 pounds,” Agwu says. “So there’s a gap between toddler age and when children reach a certain weight, making them eligible for the currently available treatments. Unfortunately, the leaky valve during that time can result in devastating right ventricular heart dysfunction or dilation.”
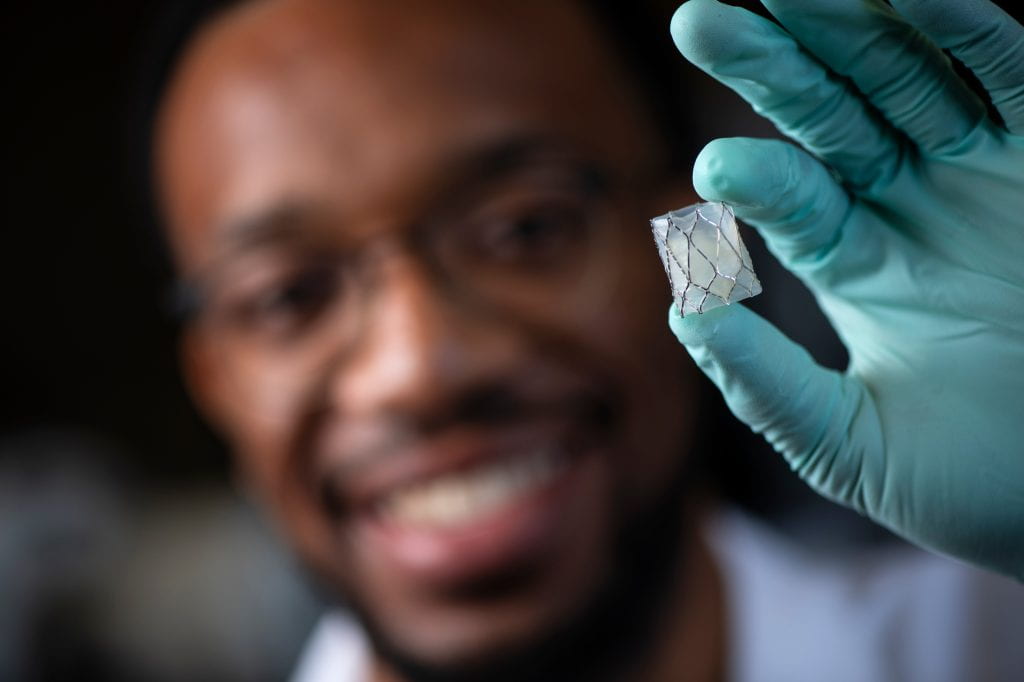
Agwu has been instrumental in the Kheradvar lab’s invention of a minimally invasive pulmonary heart valve that can be enlarged as children and their hearts mature. Designed for patients as small as 17 pounds, the Iris Valve can be deployed at its minimum diameter size of 12 millimeters and then, as the child grows and his or her blood flow demands increase, be balloon-expanded in increments up to its maximum size of 20 millimeters.
Avoiding open-heart surgery, the Iris Valve is folded and implanted through the femoral vein using the smallest transcatheter delivery system, which has a 4-millimeter diameter and is referred to as 12 French. Kheradvar says that when closed, the Iris Valve looks like the Mercedes-Benz three-pointed star logo.
“It’s crucial for the valve to be competent, meaning that when it’s closed, it should stay closed without any leakage,” he says. “In a typical transcatheter trileaflet heart valve, such as those commercially available, there is only one specific size where the valve resembles the Mercedes-Benz logo, indicating competency and no leakage. If you apply pressure circumferentially to the valve stent, the three-pointed star will twist – what we call ‘pinwheeling’ – and if you expand it radially, it will leak.”
Kheradvar explains that his team’s contribution was to invent a replacement pulmonary valve that uses origami techniques to maintain its competency across a range of diameters (12 to 20 millimeters) – from transcatheter delivery to initial deployment and later expansion when the child grows. This contrasts with commercially available valves, which maintain competent at only one size, he says.
Agwu and Kheradvar have been working closely with Dr. Michael Recto, an internationally recognized interventional pediatric cardiologist at Children’s Hospital of Orange County. Kheradvar and Recto discussed the initial idea for a valve that could accommodate children’s growth in 2020. With their complementary expertise, they transformed a concept sketched on a piece of paper into a heart valve that remains functional in animals as they grow.

“Nobody has taken this approach, to the best of our knowledge,” Kheradvar says. “Initially funded by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, we achieved significant in vivo success by implanting the Iris Valve in seven Yucatan minipigs over a six-month period.” He adds that next steps will involve extending animal studies and proceeding with the Food and Drug Administration approval process for the first in-human implant.
Positive response
The Iris Valve has garnered attention within the community of scientists and physicians focused on treating congenital heart defects. Agwu, Kheradvar and Recto presented the results of their studies at the Pediatric and Congenital Interventional Cardiovascular Society in San Diego in 2024. The UC Irvine researchers also spoke at the American Heart Association Scientific Sessions in 2023 and 2024, the 2023 World Congress of Pediatrics, and the 2024 meeting of the International Society for Applied Cardiovascular Biology, where Agwu was given the Allan Callow, M.D., Ph.D., Young Investigator Award.
Agwu’s academic background seems to have put him on a steady course to this achievement. After earning a B.S. in bioengineering with a specialty in medical devices, combined with a minor in mechanical engineering, he went to work at Medtronic and a smaller medical device firm.
“I gained experience working in both a large and a small company, with plenty of opportunities to interact with people at various levels,” Agwu says. “I got to ask a lot of questions and learned a great deal about medical device development and regulation, and I began to see what my interests were and where I would fit within this space.”
After about two years, Agwu sought a master’s degree at Missouri’s Saint Louis University, where he partnered with a neurosurgeon at Washington University in St. Louis on a device to help abate brain tumors.

“This work put me into collaboration with engineers, neurosurgeons and other clinicians; it was a unique and innovative space,” Agwu says. “It ultimately led me to decide that I wanted to pursue translational research, specifically.”
He says he started looking at R1 universities – those that reach the highest level of research activity as determined by the Carnegie Classification of Institutions of Higher Education – to pursue a doctoral degree. Agwu says he was leaning toward research in the neurovascular or cardiovascular areas and soon learned about Kheradvar’s focus.
“He consistently pushes me to reach my full potential and challenges me in ways that foster my growth and development. His encouragement and high expectations inspire me to work harder and think more creatively,” Agwu says of Kheradvar. “He provides a lot of good insight in terms of how I can work on my design thinking as well as aspects of having a better understanding of medical device development, regulatory affairs and intellectual property.”
Kheradvar, in turn, says: “Nnaoma is an amazing engineer. I try to act like a coach, and he’s the player. When he’s performing on the field, I can see things in him that he can’t see himself. I’m the coach, but he’s the star.”
- Brian Bell