Early Assurance for Early Arrivals
NeoCare Innovations Technology offers a safer start for vulnerable newborns

Nov. 13, 2024 - When Dr. Caryn Bradley, a UC Irvine Health Sciences Associate Clinical Professor and CEO, NeoCare Innovations, first set foot in a neonatal intensive care unit (NICU), it wasn’t just the fragility of the preemies that struck her. It was their resilience. Breathing and feeding, which are automatic for full-term infants, can be a daily struggle for those born prematurely.
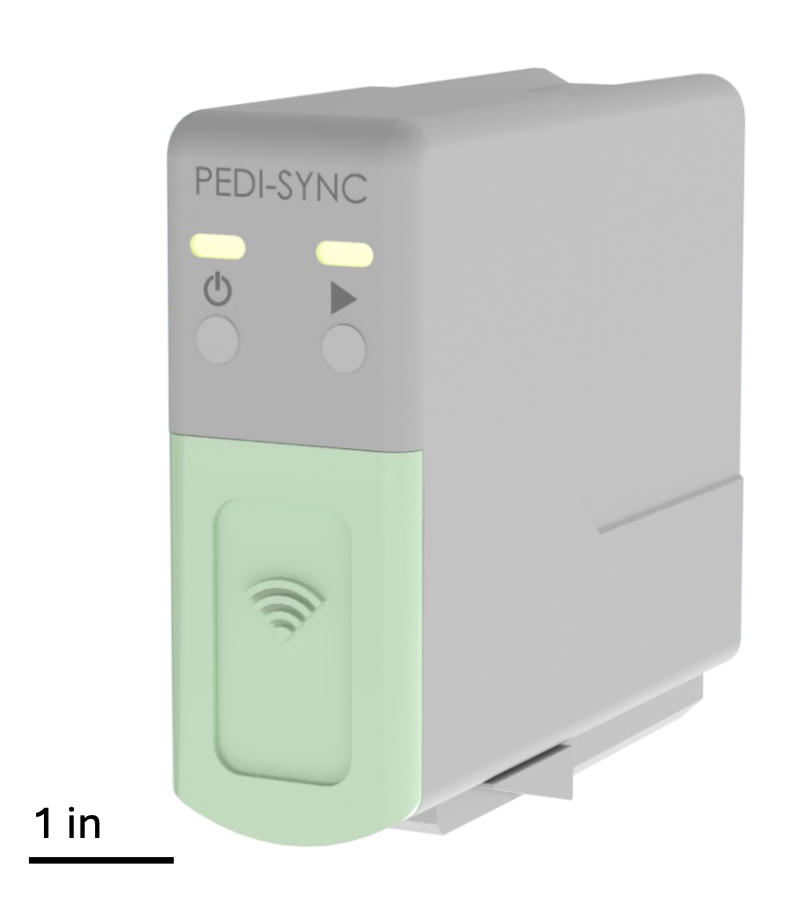
It was the desire to improve the care these preterm infants received that drove Bradley to found NeoCare Innovations, a startup focused on improving neonatal healthcare through the development of advanced medical technologies. Its flagship product, Pedi-Sync, currently in the development stage, is a clinical decision support tool designed to help clinicians assess the readiness of preterm infants for safe oral feeding. The technology uses sensors to monitor an infant’s breathing in real time. This objective data is critical for assessing whether the baby can feed safely without the risk of choking or aspiration.
“It’s incredibly scary for parents when their baby is in the NICU,” says Bradley. “Feeding their child is something they’ve been waiting for, but it’s also challenging. By giving parents objective data that confirms their baby is feeding safely, Pedi-Sync reassures them at a time when they need it most.”
Approximately 400,000 infants are born prematurely in the U.S. each year. Of these, 80% struggle with the act of feeding, which is often the last hurdle they must pass before they can be discharged from the hospital. The current standard of care—observational assessment of feeding readiness by NICU clinicians—has its limitations. Adding objective data to measure how well an infant coordinates breathing while feeding, may result in shorter hospitalizations.
“When babies can’t feed safely, it extends their time in the hospital, which is hard on both the babies and the families,” says Bradley.
By offering clinicians a more accurate view of an infant’s breathing patterns, Pedi-Sync may reduce the risk of complications and shorten a preterm infant’s hospital stay, ultimately leading to better outcomes for both babies and their families.
This innovative tool is the culmination of years of careful observation and research by Bradley and her team.
“The thought process was progressive,” she says. “It started with the babies and families. I saw a clinical need and felt we could find a way to improve patient care.”
Bradley’s in-depth understanding of the physiology of breathing and oral feeding in preterm infants, led her to hypothesize that there might be a measurable relationship between breathing patterns and feeding success. Over the years, she has gained a deep understanding of the complex issues preterm infants face, especially the critical role that feeding plays in their development and discharge.
Realizing this vision was anything but a solo endeavor. The tool required a blend of clinical, engineering, and data science expertise. UC Irvine pediatric pulmonologist Dan Cooper encouraged Bradley to build an interdisciplinary team, a step that proved essential in turning Pedi-Sync from concept to reality.
In 2018, Bradley met William Tang, UC Irvine professor emeritus of biomedical engineering at a Capstone Senior Design class, an event at UC Irvine Beall Applied Innovation where engineers could connect with faculty who could provide opportunities with their research projects. Tang’s extensive experience in engineering, particularly in medical technology development, is helping to transform Bradley’s vision into a future market-ready product. Tang is now the Chief Technology Officer at NeoCare Innovations.
“Bill is brilliant. His industry experience and technical development skills have been pivotal in bringing this idea to life,” Bradley says.
Tang and Bradley’s work attracted the attention of other UC Irvine faculty consultants, including informatics professor Kai Zheng, who brought critical data science expertise to the table. The trio, along with lead neonatologist Muhammad Aslam, created a strong interdisciplinary team spanning UC Irvine’s medical, computer science, and engineering schools, demonstrating that complex problems are best solved through collaboration.
NeoCare’s connection to UC Irvine’s Beall Applied Innovation gave them access to resources that would guide them through early-stage development, leading to successful pilot studies and prototypes. The startup has raised approximately $1.6 million in funding to date, which has been instrumental in advancing the development of Pedi-Sync and supporting clinical trials. This funding has come from various sources, including a Proof of Product (PoP) grant from UC Irvine Beall Applied Innovation which provided the funding to develop an early prototype. NeoCare has also received seed funding from the West Coast Consortium for Innovation and Technology (CTIP) and grants from the National Science Foundation’s (NSF) Small Business Technology Transfer (STTR) program, which lead to an invitation to participate in the NSF Innovation Corp (I-Corp) program. In March 2024, NeoCare secured a prestigious $944,000 Phase II Small Business Innovation Research (SBIR) grant from the NSF. This was followed by a $295,000 Eunice Kennedy Shriver National Institute of Child Health & Human Development grant from the National Institutes of Health.
While NeoCare’s focus is the NICU, Pedi-Sync has the potential to reshape neonatal care on a larger scale. Premature infants often require longer hospital stays due to feeding difficulties, and these extended stays are costly—both for families and for the healthcare system. Early pilot results are promising. Pedi-Sync may enable clinicians to intervene earlier, potentially reducing the length of NICU stays by up to two days per infant. This could translate to up to $8 billion in annual cost savings for hospitals across the U.S. For parents, this could mean less time in the NICU and greater peace of mind.
But the real impact goes beyond the immediate clinical setting. As Pedi-Sync is implemented in hospitals, its consistent and objective data could help establish standardized best practices for neonatal feeding assessment, which is greatly needed in the field.
Bradley’s work has also garnered recognition from the FDA, which accepted Pedi-Sync into its Safer Technology Program, an initiative designed to fast-track innovations with the potential to significantly improve patient care.
Upcoming pre-clinical trials at UC Irvine and another renowned medical center aim to further validate the technology, bringing it a step closer to widespread clinical use. The team’s ultimate mission, however, remains the same: to improve the lives of premature infants and their families.
“The goal is to have a global impact. We want to help as many babies and families as possible,” Bradley says.
What makes NeoCare and Pedi-Sync special is not just the technology, but the heart and dedication behind it. It’s about more than just data points or sensors—it’s about giving parents the confidence that their baby is ready to take that next step, and giving clinicians the tools to make informed, clinically significant decisions. For Bradley, that’s where the true reward lies.
“You’re not just working with fragile babies—you’re working with miracles in the moment. It’s an incredible feeling to know that something we created can help guide these tiny infants home,” she says.
- Jill Kato, UCI Beall Applied Innovation