NIH Funds Stroke Recovery Device
April 22, 2019 - More than 7 million people in the U.S. alone are stroke survivors. Stroke can leave its victims with ongoing deficits, including one known as foot drop, which affects up to 60% of those who have suffered a stroke. The patient cannot lift his/her foot toward the ankle completely – a process called dorsiflexion – which results in a compromised gait. Two Samueli School researchers are part of a team that is developing a rehabilitative tool that they think can help patients reestablish important brain-muscle connections and relearn proper dorsiflexion.
The team includes biomedical engineering professor Zoran Nenadic and David Reinkensmeyer, professor of mechanical & aerospace engineering and anatomy & neurobiology; and clinical neurologists Dr. Steven Cramer and Dr. An Do, who leads the effort. The researchers received a five-year, $3.8 million grant from the National Institutes of Health to investigate the effectiveness of their electroencephalography (EEG) brain-computer interface and functional muscle stimulator.
“Dorsiflexion is a necessary movement to walk normally and not drag your foot,” says Nenadic. “It seems like a minor inconvenience but it’s actually a fundamental part of the gait cycle and it affects patients’ lives significantly. Years of research have failed to solve this problem.”
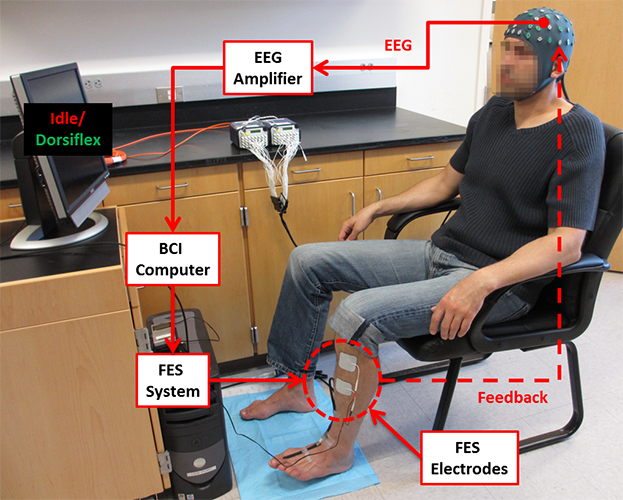
The device includes an electrode-laden elastic cap, an amplifier that magnifies brain signals and sends them from patient to computer, and a functional electrical stimulator, which attaches to the patient’s tibialis anterior (shin) muscles. Electrodes in the cap capture and send brain waves through the amplifier and into the computer as the patient, who is watching the computer screen for prompts, tries to dorsiflex. Algorithms recognize the specific brain waves tied to dorsiflexion, and as the patient attempts this movement, the device sends electric signals to his/her leg muscles.
That direct stimulation causes the patient’s foot to dorsiflex. It also sends an electrochemical signal called an action potential back to the spinal cord, where the signal meets the patient’s brain wave signals. This meeting and activation of the peripheral nervous system with the central nervous system can lead to positive outcomes, says Nenadic.
He and Reinkensmeyer believe that simultaneously activating the brain and nervous system can lead to a “rewiring” at the spinal cord and/or motor cortex level, and they are optimistic that this can inspire the brain to reestablish the missing connections. “It’s well known in neuroscience that when you have two action potentials coincident at a connection, it makes the connection stronger,” adds Reinkensmeyer.
A prototype of the device was developed in 2015 for a previous study, which found it safe for rehabilitative use. Now, researchers plan to miniaturize the device and conduct a clinical trial with stroke patients that compares the device’s efficacy to that of traditional physical therapy and later, robotic therapy.
“One of the scientific questions we’re trying to answer is ‘do you need electrical stimulation of the muscle?’ which a robot does not provide,” says Reinkensmeyer, who has previously developed hand and arm robots.
“We’re really interested in learning whether that sensory information coming back to the nervous system from your limb really matters. There’s a really big part of the brain dedicated to sensation for the hand, so it will be interesting to see if the same principles apply to the foot.”
If there is improvement in dorsiflexion, researchers want to better understand the reasons.
Reinkensmeyer says improvement could be caused by plasticity in the spinal cord resulting from the action potential flowing backward from the muscle, or it could be the result of brain plasticity caused by the sensory simulation of the muscles themselves. They hope to be able to “tease apart the mechanisms of improvement,” says Nenadic.
In the clinical study, researchers will measure patients’ dorsiflexion abilities before, during and after the patients have used the device several times a week for about a month. Patients’ abilities will be measured again three months later.
One goal of the study is to determine which patients will benefit most from the device. Researchers will compare certain stroke features and measurements before therapy begins to see if they can predict which variables will indicate success.
“If we are successful,” says Nenadic, “patients could have improved ability to walk after stroke, which will increase the social reintegration of this patient population.”
- Anna Lynn Spitzer